As you will have seen, I have been sharing maternity experiences on this blog from women I know. Some good, some bad, some unacceptable. But all anonymous. And it occurred to me that this was somewhat unfair on the birth professionals working to support pregnant women, many of whom I have become friends with on Twitter. So I thought it would be good to be able to share the other side of the story, the thoughts and views of the birth professionals, who have also been afforded the luxury of anonymity. Thus the #MatExp survey was born!
As with everything I do, I JFDI it one evening (thank you for that phrase Florence Wilcock!) and popped it up on Twitter. To my great delight, I have had 150 responses from midwives, student midwives, independent midwives, doulas, obstetricians, anaesthetists, antenatal teachers and other birth professionals. Thank you to everyone who has taken part, your input is much appreciated.
This is the split of respondents:
We also had responses from a neonatal registrar, a perinatal psychiatrist, three midwifery lecturers / educators, a research midwife, two hypnobirthing instructors, an anaesthetist and three antenatal teachers. Many are new to their profession, many have been supporting women for one, two or three decades, and one respondent has been a birth professional for 43 years.
The first thing I wanted to know was “What is the best thing about your job?” The vast majority of respondents talked about the women they work with and being able to support them as being the best part of their role. One student midwife caught the general mood with the comment “Supporting women and being there for them no matter what.” Responses included:
“Witnessing the women I support find their strength and power. Witnessing the love between the couple and the birth of a new little family.” (Doula)
“Being a part of a woman and family’s journey into parenthood.” (Independent Midwife)
“Being part of the transformation of woman to mother” (NHS Midwife)
“Supporting and empowering women, whatever the outcome of their pregnancy” (Obstetrician)
“Making a difference to women. To be present & witness to most beautiful time in life” (Student Midwife)
“Seeing women empowered and birth partners knowing their role and both having calm births” (Hypnobirthing Instructor)
“Privileged to be part of the miracle” (Obstetrician)
Unsurprisingly, the independent midwives found that being able to offer continuity of care and build a relationship with the women they support to be one of the best parts of their job. Many of the obstetricians felt that the best part of their role was “averting danger”, “saving lives”, “helping women to have as healthy a pregnancy and birth as possible”, but also “working with women caring for them at such a life changing moment in their lives” and “being able to reduce anxiety with appropriate explanation”. A fair few of the doulas talked about “witnessing the women I support find their strength and power” and “empowering women”. One explained that the best part of her job is voluntary work “with vulnerable women – asylum seekers, poverty, isolation – who may not otherwise feel worthy of advocacy”.
The word “support” comes up a lot in the responses of NHS midwives, and wonderful comments such as “Making a special time, simply awesome!!!”, “Having the honour and privilege of being a part of a very special time in people’s lives” and “working with the women through an amazing experience”. The student midwives made similar comments, but I particularly liked these two responses:
“The list is endless, but one that currently stands out is being able to turn it around when a woman is panicking in labour and giving them confidence in their own body to give birth! Saying a few words of reassurance and visibly seeing the change is incredible.”
“Supporting women on their journey whatever their circumstances or choices and feeling a sense of fullfillment when you know you’ve made a difference to someone’s pregnancy/birth.”
So from these inspiring comments from people who clearly adore their jobs, we move on to the question “What is the biggest challenge currently facing your profession?” Overwhelmingly the response was NOT ENOUGH MIDWIVES! My recent blog post explores the experience from a woman’s point of view when a unit is short staffed. This really is the biggest challenge as far as these respondents are concerned. Closely followed by fear – “The fear of litigation and professional accountability. The wake of the kirkup report savages midwives and their portrayal is unfair. We may all be tarred with the same brush. Normality is under attack again.” For midwives, morale is also a concern – “we are CONSTANTLY being told what we are doing wrong. Such a culture of fear.”
For obstetricians the challenges are different. Comments included:
“Letting the lawyers decide what information we say and letting them take an additional cut. When the press report a 5.2 million payout the lawyers award themselves a further 6 figure payout.”
“More and more ‘high risk’ women embarking on pregnancies.”
“Too much focus on everything EXCEPT caring for patients!”
“Unnecessary obstetric intervention”
For doulas, they are struggling with a lack of awareness of their role and “dispelling the myth that only the wealthy can afford us”. Lack of awareness from families – “People understanding what support we can provide and the value of it” – and from medical professionals – “Being misunderstood – doulas work alongside NOT in place of HCP”. Some respondents even felt that there is resistance to doulas amongst the medical community.
Where student midwives are concerned, the biggest challenges include:
“Feeling left alone and overwhelmed when its busy because my mentors are rushed off their feet.”
“Bullying… NHS culture”
“Working with midwives who don’t use up to date evidence such a optimal cord clamping”
“Guidelines that seem to have very little evidence base.”
“Bad attitudes, both to those in our care and to each other!”
The over-medicalisation of birth was also mentioned by many respondents.
So what can birth professionals do to meet these challenges? The #MatExp campaign is all about action, and everyone being able to make a difference. Respondents were asked “What do you feel you personally can do to face that challenge?”
Whilst some said “not a lot”, “not sure” and “nothing”, most felt that they had ways to meet the challenges they faced. Answers included the simple “keep on caring”, “keep going” and “raise awareness”. Others said:
“By empowering women to have a voice and question these [hospital procedures]. Also, working together with OBs and MWs to also understand their point of view and what challenges they face. So we can all change this together.” (Doula)
“With 3 colleagues I have set up a social enterprise to provide a caseload midwifery service through NHS commissioning at tariff – the battle is to get it accepted by those who resist changing the status quo” (Independent Midwife)
“Keep going, keep trying to provide compassionate, excellent, evidence-based care, serve the women in my care as best as I can doing my best every shift” (NHS Midwife)
“Not resign myself to that’s how things have to be, think about ways to improve and make suggestions, continue to make every contact with women as positive as possible” (NHS Midwife)
“Show by example how important it is to respect and listen to a woman at all stages of antenatal, labour and postnatal care.” (Doula)
“Ensure that I act within my own values despite others in my environment, find support and positivity from like minded individuals. I love Twitter for that!” (Student Midwife)
“Train our midwives to the highest level to avoid litigation. Test their knowledge to ensure they’ve learned from the training. Keep on asking for more staff and bigger units. Never give up!!” (NHS Midwife)
“Trying to individualise care and support women’s choices Positive birth” (Obstetrician)
“I need to remember I’m a student and should be supernumerary. I need to speak up more to make sure I’m learning each day rather than doing what I know or making beds.” (Student Midwife)
“Continue to practise in the best interests of women rather than defensively and vote against abolition of supervision” (NHS Midwife)
“Try as far as possible to support ‘normal birth’, educate women about the risks of high BMI pregnancies etc.” (Obstetrician)
“Be prepared with an abundance of solid evidence” (Student Midwife)
“Keep my heart strong, separate the bigger picture from the day to day interactions of care, do mindfulness, be compassionate to self, inspire trust in women’s bodies” (Student Midwife)
On a personal note, I particularly like the doula who is determined to be “rigorously evidence-based, and relentlessly compassionate.”
I was keen to see how many of the respondents were aware of the #MatExp Campaign. Many would be of course as the survey started out being publicised to people I knew on Twitter, many of whom I have linked up with due to #MatExp. It gradually worked its way out of that community though, and by the time the survey closed the split was as follows:
The orange line is “I have heard of it but don’t know a lot about it”.
I then outlined the aims of #MatExp as they appear on the NHS Change Day website
The next question was “What do you feel you can do to support these aims?” Many respondents felt that renewed or continued work with their MSLC (Maternity Services Liaison Committee) was the answer. Others simply want to “spread the word” and “let mums know”. Other comments included:
“I encourage women to speak up about things they’re not happy with. Raise it at a higher level if you have to, use the SoM or similar. Empower women so they don’t feel intimidated by professionals telling them what they are and are not ‘allowed’ to do.” (Doula)
“Ensure patient feedback is received acknowledged and acted upon. Continue daily ward visits” (NHS Midwife)
“Support AIMS [Association for Improvements in the Maternity Services]” (Independent Midwife)
“Keep banging the drum for parity of esteem for maternal mental health” (Perinatal Psychiatrist)
“Keep raising awareness on Facebook, hold antenatal classes, tell all the women I come across everything is in their power – try to banish the word ‘allow'” (NHS Midwife)
“Probably the friends and family questionnaires would help and I can make sure these are handed out.” (Student Midwife)
“As a researcher I can help to make maternity service user views more visible and I am also doing a lot of work around ways to increase opportunities for service users to get involved in research/maternity service improvement activities. I am also very interested in the idea of co-creation in research (so working alongside service users and frontline staff to develop, do and use research). Part of the work I am involved with at the moment involves empowering pregnant women and midwives to use research evidence more effectively.” (Research Midwife)
“I’m an increasing Twitter user. Social media seems to be the way forward” (NHS Midwife)
The next question looked at the specific areas that the #MatExp campaign covers, including the area for which I am one of the champions: “Life with a new baby”. The full list is:
Skin-to-skin – see Jenny Clarke’s video
Optimal cord clamping – meet Amanda, optimal cord clamping champion
How does lithotomy feel as a woman in labour – read about obstetrician Florence Wilcock’s NHS Change Day lithotomy challenge
Language used towards pregnant women (e.g. “failed induction”, “poor maternal effort”) – this area is championed for the campaign by Leigh Kendall
Life with a new baby – including perinatal mental health and breastfeeding. Read about Rosey PND&Me and also the blog post that Emma Sasaru and I put together on supporting breastfeeding.
Informed Choice – see this example of risk being explained in a user accessible way
Respondents were asked to rank these areas in order of importance and the results were:
A couple of respondents had (very fair) specific comments on the above question, namely “our unit is already changing skin to skin and delayed cord clamping, hence their low ranking, otherwise I would have placed them higher, my next project is to reduce the use of lithotomy” (Obstetrician) and “it is impossible to rate these in order. In general they each impact on each other, by improving informed choice you are creating a healthier postnatal environment etc. so rankings don’t mean that skin to skin is the least important” (NHS Midwife).
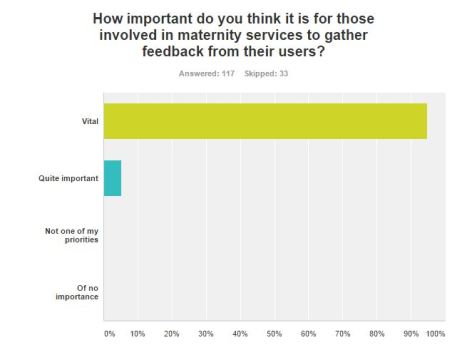
The response to the next question was fairly definite!
Finally, I asked “If you could change one thing about maternity care in the UK what would it be?” Staffing levels were mentioned again by a lot of respondents, as was caseloading / one to one care. Many of the answers were also indicative of the tensions between different birth professions and professionals:
“For more medical staff to witness natural birth.” (Doula)
“Doctors and midwives respecting each other” (NHS Midwife)
“Obstetricians” (NHS Midwife)
“If we loved and treated our colleagues better, collaborated and supported each other, we’d be a happier, more efficient more compassionate and passionate workforce- and this would filter through to the women we support” (NHS Midwife)
“Reduce obgyn lead care.” (Doula)
“NCT didn’t have such a negative influence on women. No one failed because they didn’t have a vaginal birth. A lot of what is taught is inaccurate and based on personal opinion which is not informed choice.” (NHS Midwife)
“Slow down the relentless overuse of induction…encourage/ optimise midwife led care home birth and birth centres and caseloading model of care.” (Student Midwife)
“Don’t always go and try to enforce your procedures. Listen to women. Use of language for the purpose of influencing a labouring woman into accepting the best thing for hospital such as I witnessed: ” This baby has had enough” is very detrimental, and to say the least, manipulative.” (Doula)
“I would offer a single additional session to antenatal classes/NCT classes etc about the reasons for medical interventions in labour and the risks and benefits. It is unbelievable that in an age of information, when women have spent time with midwives and NCT instructors, we still regularly see birth plans that say “don’t want forceps unless necessary”! It immediately disadvantages obstetricians and puts them on the back foot, as we not only are seen as “the bad guys” for forcing these interventions on women, but often have a matter of minutes to explain the risks and benefits in an urgent situation, which is frankly laughable. Obstetric trainees should be involved in antenatal education; just a single group session on the what, when and why of CTGs, forceps, FBS and Caesarean would I think remove a lot of the fear from women and help those for whom labour does not progress smoothly to feel more empowered and informed.” (Obstetrician)
“More trust in women to make the right choices for themselves. Less bullying and misinformation.” (Independent Midwife)
“Obs and midwifery attitudes to each other.” (Anaesthetist)
I would also like to highlight this heartfelt plea from an NHS Midwife: “I don’t even know where to start… Let’s be compassionate again – let’s treat EVERY woman like our sister. Even the smelly, rude, unpleasant ones. Let’s try.”
Along with a number of #MatExp participants on Twitter, I have been saying that respect and compassion are two vital elements of a positive birth experience, regardless of vaginal birth, c-section, place of birth and so on. This comment from a doula certainly chimes with my personal view on what could change in UK maternity care: “I’d like it to be less of a lottery, some professionals are kind, supportive, informed, happy to discuss options with women. Some are not. On the same wards, in the same hospitals too. I’d like the good experiences that many have to be normal for all. The feedback I get is this comes down to how the woman is treated rather than the final outcome of the birth experience.”
The full results of the survey have been passed to Florence Wilcock, #FabObs of the #MatExp campaign.






Thanks Helen for this, it’s great to hear other perspectives. Some parts a bit depressing (what do you think needs to change? – “obstetricians” – right! Nothing like a we/they siege mentality to get things off on the right foot!) but encouraging that we all seem to be there for the same reasons, ultimately want the same things for women, and are (mostly) keen for more inter-professional support and respect!
I’m interested by one of the comments regarding language; someone is clearly very against “your baby has had enough”, which I’ve said on occasion I’m sure. I would usually talk in terms of “tiredness”, because throughout contractions, CTG decelerations (which can be very worrying for women who understand “their baby’s heartbeat is dipping”) I try to explain in terms of exercise/swimming, the baby having to hold it’s breath, having time to recover etc.
Surely saying the baby “has had enough” is better than “we’re worried your baby isn’t coping/is struggling to compensate/may be becoming oxygen deprived/is distressed” etc?! What are the doula-approved ways of communicating concern for fetal wellbeing?
LikeLike
Thanks so much Tom, thank you for reading it. I may be wrong, but I think that doula comment was suggesting the phrase was used as a way to manipulate the mother into doing something the doctor wanted, without that “something” being necessary. In that situation, the choice of language seen as manipulative. Like I say, I might be wrong though – will ask some doulas to comment. H.x
LikeLike
Hi Tom, thank you for commenting here, it is lovely to see some joined up working within #MatExp. With regards to language, maybe talking realistically to mum about what is expected of baby at certain stages of labour and if there is a problem, why you think it is a problem, ensuring a clear conversation is had will help. Simply stating “Your baby has had enough” is negative language and could potentially leave women feeling deflated and that they have let their baby and themselves down by opting for their chosen birth path. If women understand your concerns and are given true informed choices, relationships between all may work out for the better and open dialogue can occur. Hope that helps a little. Nikki @TheDoulaElement
LikeLike
I was asked for my thoughts re. Tom’s comment (I’m a doula, amongst other things).
I like Tom’s suggestion of referring to tiredness and explaining in terms of exercise. I agree that actually, it comes down to taking the time to explain what’s going on in a way that a woman can understand without causing her a lot of concern – so, yes, explaining that her baby might be becoming tired (rather than her baby’s heart rate is dipping, becoming distressed etc.), it’s not a panic situation, so let’s start having that discussion now about options – the pros & cons of those etc.
The phrase “your baby’s had enough” does sound very negative and alarming – it sounds like her baby is just going to ‘give up’ and that’s that! Just as alarming as “your baby’s becoming distressed/ his heart rate is dipping” etc.
In all this I’m assuming that it’s not a crash situation and that there IS time for discussion. In which case it just takes a little bit of thought to ensure language used is less negative, and obviously more time – doing the explaining etc. above will take a bit longer than saying “your baby’s had enough” but could make the world of difference to how parents will feel in that situation.
LikeLike
Thank you for commenting Louise. An important #MatExp discussion – language vital. H.x
LikeLike
Coming to this a bit late, but a lot of what is said above echoes with me. With the original comment, we cannot know the circumstances under which it was said – it might not even have been a baby in distress! But, yes, I feel that saying “the baby has had enough” is both negative and is also forcing an opinion on a situation. That baby might be fine, might cope longer even signs are not perfect – you do not KNOW. If you say “I am concerned that your baby is getting too tired” that is truth. It is your opinion of the situation right now, stated as such. That gives the parents accurate information to make the decisions THEY feel are right. No one else can make decisions for parents, unless they are declared incompetent or there is a true emergency with no time for any discussion in order to save lives. I have seen multiple instances of OBs (particularly registrars) speaking like it is their responsibility to make decisions for couples. No. Give them the best information you can, which might include your opinion but stated as such, then let them make their decisions. I do wonder whether accepting that these are often not their decisions to make helps more senior OBs I have known who seem more relaxed??? Hope that helps. I’m very not a “them and us” kind of person!
LikeLike
Hilary Pengelly (doula) would also like to comment here. She struggled with the website comments section, so has asked me to post this on her behalf:
“Hi Tom,
With my doula hat on, and other hats I have worn (!) I feel it is important to facilitate communication between the woman/her partner and her birth team, so that her choices about her labour can be heard and responded to with respect; as a doula I try to do this. I agree respectful interprofessional communication matters too, but ultimately this is HER birth.
So yes, the labouring woman needs to be given clear information about her situation and her baby’s wellbeing, but the language used to convey this impacts on how she experiences her labour, and how confident she feels about birthing her baby. A phrase like ‘your baby has had enough’ is emotive, and could undermine the woman’s confidence or make her feel a failure. It can imply she’s had her chance, and now someone else needs to step in to safely deliver her baby.
Unless this is an emergency, it’s possible to take the time to explain in a clear, factual way what is happening, and what this may mean for both mother and baby. It’s about trying to promote respectful dialogue between the woman and her team…helping her to understand your concerns, and really listening to her(s).”
LikeLike
Wow amazing post with so much inforation and it is really great to hear from the professionals themselves about how they feel about the job they do and what can be done to improve it. Glad to see respect and compassion feature so highly, as that would make a lot of difference to a lot of women! Thanks for linking with #MaternityMondays
LikeLike
This is so interesting! And for me to see how the professionals feel about it all, There does seem to be a dinstinction between midwives and doulas and doctors. The fact that doctors found high risk pregnancoes challenging spoke volumes. That was me, but I never saw myself that way. Its so hard to see myself that way!
This is such a wonderful way to get a true reflection of how things are at the moment, and it will be really interesting to see what the answers are in 12 months time.
Thanks so much for linking up to #MaternityMatters x x x
LikeLike
It’s lovely to see the prominence of SUPPORT as the aim of maternity care professions, and it’s so interesting to see the differences in the challenges they face. I agree that an NCT antenatal class from obstetricians about medical interventions during labour is definitely a good idea; it will take the fire out of the fear that comes with it when thinking about a birth plan. I’m pinning this for future reference. Thanks for what you do. #MaternityMondays
LikeLike
Thanks for reading 🙂
LikeLike
Wow as an New NCT Practitioner I am still shocked by the negativity about our organisation from other HCP. I accept that an additional session could be useful, whether in NCT Session, hospital or in a community venue. However you can not blame the NCT for every women who has decided to write a rigid birth plan or not understood or taken on board the information discussed in classes. Adults are in control of their own learning and what action they take going forward is not always an accurate reflection of the NCT, it’s practitioners or sessions/classes. What I personally try to do is empower women to ask questions, to be informed and trust herself and her baby. I want to work with midwives and OBs not against them and I am sick of being tarred with a brush of outdated opinion. Lets work together to give women and their partners a better experience.
LikeLike