I am starting a new series of blog posts today about health visiting and the relationship between health visitors and parents. This is something that I became concerned about over a year ago, having seen numerous posts on my Facebook group about questionable advice from health visitors, HVs upsetting mothers, a lack of health visiting support and so on. My family has been so fortunate in the wonderful support we have had from Anna Embleton and the Sale Moor health visiting team, it saddens me that this is not everyone’s experience. It is also a concern, as if parents are losing faith in HVs then it will be that much harder for health visiting teams to communicate important public health messages and provide support to families.
This becomes even more of a concern when we consider the changes that are coming this October, when health visiting will start to be commissioned locally instead of nationally. If families do not value their health visitors, will there be enough public pressure on local authorities to commission the services that communities need?
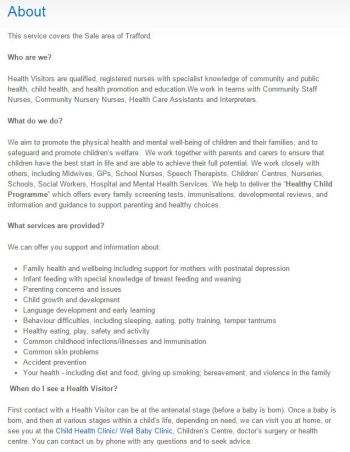
Health visitors currently work to what is termed the 4, 5, 6 model, which is 4 levels of service, 5 universal health reviews and 6 High Impact Areas.

So what feedback have I received on social media about health visiting advice over the last year or so, particularly in relation to the areas covered by this model?
Universal Health Reviews
“Mine saw baby at 3 weeks and hasn’t seen her since – she’s now 7 months! Not even a phone call!”
“My little girl is 6 months old and I’ve only ever seen my HV once, and that was when she was 10 days old.”
“My current HV told me she’d come out to see me at 6 weeks post birth – 6 weeks has been and gone and I’ve heard nothing. Good thing there are no issues!”
“I can’t even remember a thing about mine…..they stop coming at about 6 weeks don’t they? I vaguely remember having to be in for when someone was coming but can’t really remember what they did. Babies are 20 months now so it seems a long time ago.”
Transition to Parenthood
“My HV advised me not to go to any groups until my daughter had received her first set of injections. As I was new to it all I didn’t go to any groups until after the first jabs. Which was hard. When I did start going to groups the Children’s Centre were shocked and told me this wasn’t the case at all. I believe that the Children’s Centre were rather upset as they want to get as many mums & babies to the groups. It was reported to a higher power but I’m not sure whether the HV was advised of the correct procedure.”
“I had had an episiotomy and I asked whether the stitches would be checked at some point. I’d had surgery / stitches on my foot prior to being pregnant which had had regular follow ups. I assumed, given the ‘vulnerability’ of the area in this case that someone at some point would want to make sure they were ok. Want to know what my HV said….?! ‘well not everyone wants to get on a table, spread their legs and show someone their vagina.’ “
“I find like any professional you get good and bad ones. What does annoy me is the inconsistent advice you get from them. I rarely see the same one at baby clinic and they all have a different opinion on things which just leaves me confused about what’s best for baby!”
“With my little girl we were seeing the doctor for weighing on a monthly basis due to her reflux. On the two times I visited the HV for weighing they didn’t listen to the reasons why she wasn’t putting on a massive amount of weight or that the doctor was seeing us. They made me feel stupid and like I wasn’t caring for my child by insisting that she needed to be seen by the GP straight away and that the GP’s recordings were wrong. I just stopped going. My daughter still hasn’t had her two year check and will be 3 in August.”
“Any HV I’ve ever come across has been very reluctant or unable to answer any questions directly. Seemingly for fear of being blamed if something goes wrong based on their advice. One that I asked about the amount of milk needed at 8 months, and for tips on getting baby off the breast and onto a bottle, told me to go and talk to the breast-feeding counsellor instead about it..! I’m a bit confused as to what their purpose is to be honest. My mum’s friend is a retired HV and has said to me ‘Most babies are pretty sturdy and will grow anyway, so I just used to tell mothers what they want to hear.’ Pretty much sums up what I’ve found – except for the ones that are downright rude and make mums feel the worst ever.”
“In general I’ve been disappointed by my HV contacts, to date I’ve had 3 different staff and little support has been given. I’m not sure what I was expecting but on each occasion I’ve simply been given NHS standard literature on a variety of topics.”
“My health visitor is a bit patronising if I’m honest; leaflets leaflets leaflets I hate the text book way they work – all babies are different. I think they should see you a lot more as well on your first baby. I don’t feel as though I see mine enough – luckily I have experience with babies but for people who don’t and it’s all new more support is needed definitely.”
“I’d like it to be a bit more personal & a little less textbook, when you’ve just had a baby you’re so worried about every single thing & health visitors (I doubt on purpose) don’t make that any easier. I saw a post of a lady a few days ago saying she hoovered the entire house & even changed the bedding because her HV was coming round. It’d be nice to have that reassurance that you don’t need to do that, even if it’s just a comment “oh wow you’re house is lovely considering you have such a small baby”, maybe this would mean mum is a little more relaxed on the next visit. Also a little more interest in your own baby rather than ‘all babies’ and just being given leaflets upon leaflets of how it should be done. Mine couldn’t remember my daughter’s name once, she kept asking. I’d like to be able to have a nice chat and maybe even a bit of a laugh with the HV and I never felt comfortable enough to do that, it felt a bit like I was in an interview to be honest.”
“I’m currently on health visitor number three. My little girl is 9 months and I met the first one once before she was born. Only met the second one once too. The rest of the time it’s been another health visitor. Although they have all been helpful and supportive, it’s hard to build a relationship with them when you’re seeing a different one all the time.”
Maternal Mental Health
“I never had a home visit. I got a letter when my baby was a few weeks old telling me they were busy and there weren’t enough to go round but if I wanted to see someone I could give them a ring or go to the drop in.”
“For the first 2 months my little girl would only sleep vertically, which meant that my partner and I slept and ate in shifts as she would only sleep on us – we tried everything – carrycot in cot, cot, Moses basket, swaddling – nothing worked. I was also breastfeeding. The Health Visitor was unmoving in her mantra of ‘baby must sleep in her own bed, baby must not sleep with us’. It was really stressful. I was sleep deprived. Terrified I was doing something wrong. Scared to admit to my depression as I thought they would think I was incapable etc etc. In the end, after weeks of this I straight out asked her what she would do and she couldn’t give me an answer.”
“Went today & had to fill out a questionnaire about post natal depression. I scored 12??? Whatever that means but I always feel they judge me. I’m absolutely fine & happy, but like any new mum have tough days. Going today has made me feel more down.”
Breastfeeding
“At the time, I couldn’t understand why the HVs I saw refused to give me any kind of support, or tell me where I could get it. Now, I realise that they had no idea what they were doing, were understaffed, under-trained, and trying to get through too many appointments. They were resentful of their working conditions and taking it out on the women they saw. Visits were purely about getting through the paperwork they needed to show they had done, and nothing else. In my opinion they did my daughter and I a lot more harm than good, which is why I am going to give them one chance only to impress me this time. In their favour, they didn’t put as much pressure on me to formula feed as the community midwives did, but only because they didn’t really say much at all.”
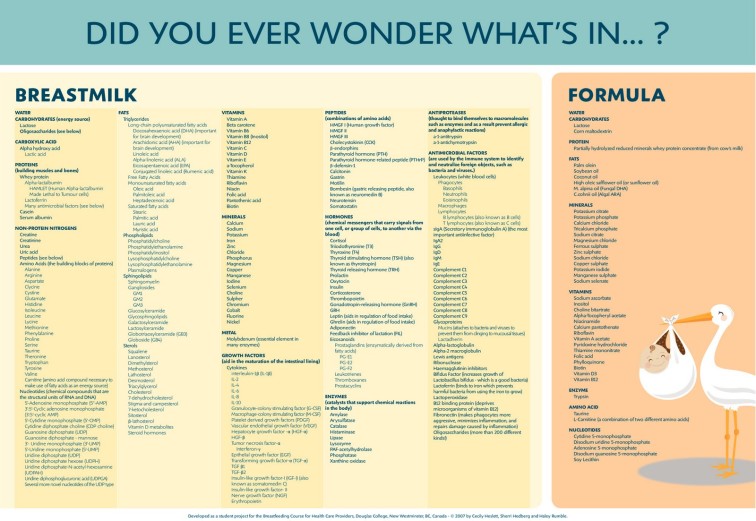
“I had mixed experiences. Judging by the huge number of moans on the many breastfeeding and parenting groups I am part of, in general people find their HVs to be unhelpful and giving inaccurate information. Of course, there are some great HVs, but wouldn’t it be good if they were all as good. With regards to breastfeeding, I believe that many HVs are not educated enough in the art of lactation! (The same goes for doctors, nurses and other health professionals.) They give wrong and misleading information. So many mums don’t get the help they should have and are failed by the health service. Many more would continue breastfeeding for longer if they just had some help. It is so often a regret for mums that they didn’t persevere and it is often not their fault. They just needed that support or help.
So why are HVs not trained by La Leche League or whoever to be lactation consultants? And why are they not giving out accurate and up-to-date information? Mums must of course have the choice whether or not to breastfeed, but I believe that we are not provided with all the information and the evidence about the benefits of breastfeeding and the problems with formula feeding. And then if us mums do have problems, why are we not helped by trained lactation consultants. So long as people are educated enough then they can choose to stop breastfeeding when they wish, but at the moment so many mums are being failed because they are not fully informed and so they are stopping prematurely. I truly believe that there will be a revolution at some stage against the multimillion pound advertising from the formula companies who are giving out inaccurate information about infant feeding. Once the health service starts to provide help and education, this revolution will start.”
“Definitely think HVs do not often have up to date breastfeeding info especially when baby has lost a little bit of weight; instead of suggesting upping feeds etc they are quick to suggest that your milk is not enough and they must have formula which then totally interferes with a mum’s supply often making things worse not better, and thus the downward spiral of an end to breastfeeding.”
“I am not sure why but my daughter was never an enthusiastic feeder. At the time, I felt I was being blamed for not producing enough milk. I did everything they said and even tried expressing, but I couldn’t produce any more. I fed on demand and she never wanted more. Her weight started to plateau at 5 months and we ended up having to wean her early. I broke down at a weighing session and thankfully there was an Early Years advisor there who was a breastfeeding specialist. She came and visited us at home the next day and was wonderful. For us though it was too late – I just couldn’t produce any more (tried super switching?? etc) and we decided to wean her early and use a mixture of bottle and bf when I went back to work when she was 6 months (I didn’t want to, circumstances dictated). I carried on breastfeeding for another 4 months after I went back to work full time (morning and evening). My little girl decided to stop at 11 months when she got her first cold.
I have discovered that I have seriously low levels of vitamin D, which wasn’t picked up until the end of last year. I don’t know if that had anything to do with it. I am still really upset (I am in tears just writing this down), 4 years later, that I couldn’t produce more milk, that I couldn’t encourage my daughter to take more and I didn’t get the support I really needed at the time. I really do feel like I failed her in that respect. I have no answers. It’s still so raw.”
“I’ve actually just been to the self-weigh drop-in clinic and asked about nighttime feeding. Again I was given a leaflet and told that at the age of 34 weeks my baby doesn’t “need” food during the night and we should stop immediately and only give her water to satisfy her thirst! I guess I was hoping for a little more support as a first-time mum.”
Healthy Weight
“The health visitor I used to see was lovely, very approachable, good with advice, kind and made you feel good about what you and baby had achieved together. However one week I had a stand in … absolutely horrible woman. Had no time for my little boy or to listen to what I had to say. I said that I was concerned about him not eating a variety of foods and wanted advice. None was given other than ‘put him on the scales. I’ll see what his weight is like’. Yes he had dropped a little as I had guessed and all I was told was “he’s underweight push more food”. I left feeling very upset and that I was failing as a first time mum. This put me off going to the health visitor unless I have to and also made me paranoid about the amount of food my boy eats”
“My health visitor was lovely, a very sweet woman with a gentle manner, but I have to say (not sure if politically correct to mention) that she was obviously clinically obese. This did leave me to wonder how she managed to conduct her job with regards to advising on healthy lifestyle. She did comment that my 2 year old at the time had increased quite a lot on his centile (chunky and tall but not overweight!) and that I should really keep an eye on that!!?”
Managing Minor Illness and Accident Prevention
From the mother of a child with a Congenital Heart Defect: “My HV is a very nice person, but hasn’t a clue what to do with my little girl as she isn’t ‘normal’. We have seen her 3 times in 5 years but she has said if I need anything to ring her. When I have asked her for anything she has said ask the hospital as my daughter is under them! I just didn’t bother from then onwards.”
“I voiced my concerns to my HV regarding my little boy’s back and his lack of movement in his neck and she shrugged it off and said he was fine without a second look. Didn’t even bother to make a note of it in his red book. Despite her advice I went to see my GP who made an instant referral. Then he was diagnosed with scoliosis and torticolis. Glad I followed my instincts! It has made me lose faith in my HV.”
“My health visitor told me that because I am in a same sex relationship she didn’t need to worry about domestic violence, because only men beat up their female partners because they get jealous of new baby.”
Healthy 2 Year Olds and School Readiness
“Has anyone had to deal with a toddler head butting when they can’t get their own way? My little boy is 18 months and been head butting loads when he can’t get his own way. I spoke to the health visitor before Christmas and she told me to strap him in the pushchair when he is throwing a temper tantrum but I don’t want to be doing that.”
It is interesting that Infant Sleep is not one of the High Impact Areas, as it is certainly one of the areas with the highest impact on parents! This comment is unfortunately not unusual, which is frustrating considering the evidence available on infant sleep and “sleep training”:
“My health visitors were awful, I only saw someone three times before opting out.
The last time was when my little girl was about 5 weeks old and the HV told me I should let her “cry it out” to get her to sleep… She had colic… So no, I don’t think that health visitors are helpful in the slightest.”
The above comments are a snapshot of what is a weekly if not daily subject on my group and other social media forums, and I felt that I needed to raise this with somebody. Simply trying to find out online who is responsible for health visitors is a difficult task for a parent who does not work for the NHS and so doesn’t understand the hierarchies. Should I speak to the Nursing & Midwifery Council? Should I speak to NHS England? Should I speak to individual trusts? Who decides on training for health visitors? Who can tackle perceived inadequacies?
In the end I wrote to two organisations: the Institute of Health Visiting and Unite. I have since had a lot of contact with both organisations, and other senior health visitors working for the Department of Health, and the feedback from my group has been provided to quite a few people. More of that another time. The first discussion I had on all of this was with David Munday of Unite, when I met with him at their Salford offices in December 2014.
My meeting with David was helpful and productive. He gave me some background to health visiting in the UK which goes a long way to explaining some of the issues families experience. David explained that between 2000 and 2010 there was a dramatic decrease in the number of health visitors in the UK. Caseloads in some areas went up to 1,000 families per health visitor. As a result of some awful cases that hit the news, all political parties promised to increase the number of health visitors during the 2010 election campaign. There has been an increase in the last 4/5 years, and the pledge was that there would be 4,200 more HVs by April 2015.
Click here to see #CPHVatt debating progress on the HV Plan on Twitter around the time that I met with David Munday.
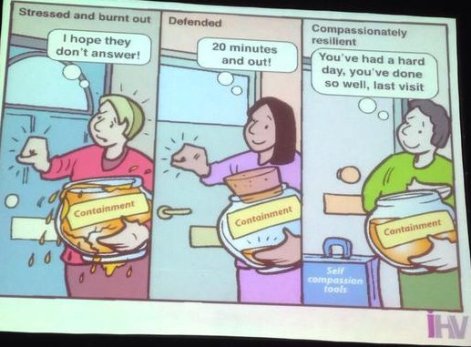
So we have a situation where the profession lost a lot of experienced practitioners, and now 50% or more of HVs are newly qualified. An exhausted profession is then being expected to train up a lot of novices.
Now, this does not excuse some of the things we as parents experience, and David did not offer it as an excuse, but it does explain why some health visitors do not have the time or inclination to keep as up-to-date as we would like them to be, or to be sunny and positive at every appointment.
Baby Friendly training is helping with regards to breastfeeding knowledge, although it will take time for the effects of this to be seen. The impact of the closure of children’s centres is huge in David’s view – and I know that in my own borough, Trafford, all but 2 of 16 original centres have been closed over the last 3-4 years. The Birth to 5 book is no longer available in hard copy, as a cost saving measure, hence the myriad leaflets with which HVs and families have to contend.
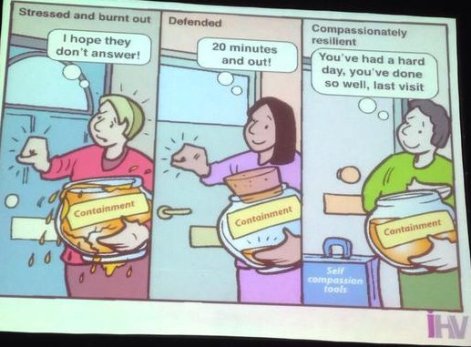
It is important to remember that health visitors have to deal with some awful situations (I know of HVs who have received death threats) and their primary concern is always the safety of a child. The profession is over-stretched and lacking in resilience – something I see frequently on Twitter, where the passion and compassion of health visitors is being pushed to breaking point. David referred to “going upstream” – when HVs are under pressure they focus on pulling out of the river the people who are drowning. In an ideal world, they would be going upstream to find and tackle the causes of people being pushed into the river.
From the Institute of Health Visiting
Since that initial meeting I have had many more discussions about health visiting quality and quantity and I will be discussing approaches, improvements and gathering feedback in later posts. For now I wanted to leave you with the other side of the coin – the positive comments that have come from members of my group. Because there are a great deal of fantastic, hard working health visitors out there doing their best for UK families:
“My HV has been fantastic, has always been very good at listening & answering any questions I have had. My little girl was the first baby she had seen with a heart defect & di George syndrome, so she spent a lot of time looking into it & getting ideas on what I could do to help my daughter.”
“I feel really lucky, mine have been good in all sorts of ways. If I’ve been worried that I’ve not heard from them when a check of any kind is due, I just phone and chase them up. We’re also very lucky to have a breastfeeding guru (not sure of her official title) in our area who is also qualified to deal with tongue ties and did so with my first son as soon as she had diagnosed it. When I did go over to formula they were also supportive and I didn’t feel judged or a failure. All good so far really!”
“Appreciate that she is one of thousands in the country, but I can only speak positively of my HV. She covers our village and the surrounding ones, so we always see the same person, she’s ready to answer any question however silly, is always at the end of the phone and willing to do home visits. She’s chased prescriptions and hospital appointments and arranged an eye test for my 2 year old immediately when I was concerned about a possible squint. Importantly, she always gives a balanced, common sense view….she has been in the job for a long time and seen lots of changes in guidance and policy….she will give the official advice and tell you why it is what it is, but also tailors her advice to the individual baby. I think if I had a young one who just took a “tick box” approach I would get very annoyed! So there are good ones out there!”
“My HV is lovely; unfortunately she has not managed to actually help much with my little boy because of his issues but she is always there to support me. The last two times she hasn’t even come to see about him, she’s keeping her eye on me because of my recent problems with coping and depression. She is very supportive of me and it’s lovely to have that from an ‘outsider’ so I have nothing but positive praise for my HV!”
“My HV was brilliant, as was the rest of the team. I was able to contact them whenever needed and when I first called up to ask for help because of suspected PND they kept me on the phone for an hour talking to me and discussing next steps to get through the night, until they could make a home visit the next day. So nice and friendly and really calmed me down and helped me. I asked her for plenty of advice on PND, baby sleep, baby eating, illness etc and she was able to provide really good advice as far as I’m concerned, it all worked at the end of the day and it’s advice I still pass on now to other mummies to make their own decisions. She was non judgmental as to our choices. She seemed very comfortable around children, and had a no nonsense approach that may have put some off but I felt at ease with that as it exuded confidence and made me trust her.”
“I have to say that the health visitors in my area have been a mine of information and support for me. Particularly the breastfeeding support I had that came out for home visits and phoned me to see how I was doing till we were comfortable with it all. And a massive support from my sleep expert lady she has been my rock when I thought I was losing the plot. No complaints here.”
“My health visitors have all been great. Really supportive when my son didn’t put on much weight the first few months and supported my decision to exclusively breast feed even though I think they thought I should have topped up with formula. Also very supportive about sleep (or lack of), I have cried on them many times, and have had a few home visits from them about it and attended a talk. However I’ve realised they don’t have all the answers and sometimes have conflicting advice, but they always give me an idea of something else to try which I’m really grateful for. Having heard bad things about HVs before I had a baby I was worried, but I have felt really supported. My son is just over 11 months, we’ve just had his check and the HV was fab and really gave me confidence that I’m a good mum, which was exactly what I needed to hear.”
“Mine was fab, to be honest just what I needed when trying to breastfeed twins with tongue ties and never once did I feel under pressure to breastfeed. My HV even sorted out some HomeStart to help once a week which has been a godsend, also she arranged for a breastfeeding adviser to get in touch with me who in turn came out to see me a few times and was a major influence in me continuing to breastfeed as long as I did.”
“I must say I really like my HV, she’s really nice and approachable and I know if I needed to I could contact her and she would come and visit. She visited more often at first as I was having breastfeeding problems. She referred me for an early days group at the local Sure Start for first time mums and she’s been really informative with advice. Last time she came was two weeks ago – it was supposed to be our last visit but I was quite tearful and emotional as I was tired and worn out as my daughter had started waking in the night again. It was “just one of those days” but I think she could tell there was something wrong as she kept asking “are you sure everything is alright?” then I burst into tears, embarrassing! She stayed and chatted and reassured me that everything will settle and she arranged to come back to see me tomorrow to make sure I’m okay and to check things have settled.”
“I have no complaints with the health visitors I have met in Northwich or the ones that go to Cherubs in Winsford. I have found them all kind, supportive, caring and pleasant. I had breastfeeding support from them in my home in the early days. I had a trainee as well as my own HV, and whenever she sees me she knows my name and my little boy’s without a reminder which I think is lovely.”
“My second HV, Louise, was and is completely brilliant. She came round, asked how she could help and listened to me. She still filled in forms, but as part of a chat, so the form was incidental, rather than all-important. When I was struggling with anxiety, she visited weekly and then monthly until I told her I was feeling better. When she visited and I was exhausted from breastfeeding through a growth spurt, she made me a cup of tea. Little things, but they all added up. She also made it clear that she would help me access any services I needed to access. I didn’t need to take her up on it, but it was the reassurance that mattered. Louise pretty much fulfils my idea of a perfect health visitor.”